Insurance Verifications with AcupBilling
Verifying insurance is the foundation of any profitable medical billing practice. Learn how you can save countless hours with this feature.
Insurance Eligibility Verifications are the first and most important step in ensuring you are billing accurately. Full benefit breakdowns often require phone calls and the wait times can range from 20-45 minutes per verification.
Let our Insurance Verification Service save you time that you can reinvest into your clinic.
Patient eligibility verification – particularly when done in advance – ensures you have up-to-date and accurate insurance patient information and helps prevent unpaid or denied claims.
This insurance verification service was developed to seamlessly take over the burden of checking patient insurance benefits by phone before their appointment. We’ve partnered with acupuncture insurance billing experts AcupBilling to verify your patient’s benefits.
Unified Practice Insurance Verification is
- Reliable – All verifications are performed via phone by the AcupBilling team
- Seamless – This feature fully integrates with Unified Practice
- Fast – Verifications are made within 2 business days
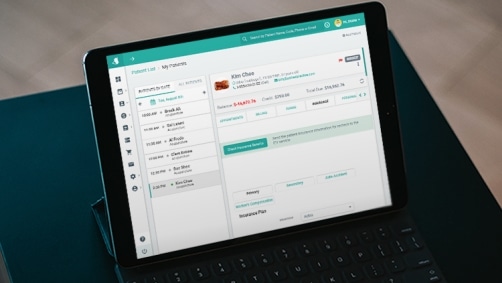
- Visible – Your verification status and reports are available real time, right on the Unified Practice dashboard
- Simple Pricing – Only $3.95 per verification, for up to 5 CPT codes.
Easy to get started

No set up or training fees

No long term contracts

Easy online form
When you put the verification process in our hands, you receive:
- Fewer surprises and greater patient satisfaction
- Ability to accurately estimate insurance and patient payment portions
- Higher/faster collections and reduced claim rejections
Pricing
$3.95 per verification - for one service and up to 5 CPT codes
Sign up today to receive your first 3 verifications for free
Frequently Asked Questions
Verifying patient eligibility is becoming an indispensable process when it comes to billing patients, getting paid by insurance providers, and the overall management of practices’ revenue cycles. With the rise in high-deductible and cost-sharing insurance plans, more and more patients are required to make payments at the time of service, though many patients are unaware of this fact. Successful billing depends on effective eligibility verification.
Once a patient’s insurance information is entered into Unified Practice, an insurance verification specialist is alerted to call the patient’s insurance company and check if the patient’s plan covers the services you offer. If there is coverage the specialist will also find out additional details such as copay and deductible amounts along with any restrictions on procedures or number of visits.
You control when and how Insurance verifications are requested, see ‘What triggers a verification?’ section below.
AcupBilling has provided acupuncture billing services to satisfied clients across the nation. They are a professional billing company with extensive knowledge and vast experience to help their clients receive the maximum reimbursement from insurance companies. Most importantly, they truly care about their clients. In their words: “We are devoted and will strive to meet your individual needs. Our attention to procedure, accuracy, and timeliness will maximize your profits, minimize claim turn-around time, minimize claim losses and reduce your office hours. We are also fluent in both English and Chinese and strive for customer satisfaction.”
Your first three verifications are FREE! Afterwards, the cost of this service is $3.95 per verification, for one service and up to 5 CPT codes. This is how pricing works: We will issue an invoice and charge your card on file at the end of each month. The pricing will be based on the number of verification checks made during that month regardless of the result of the check.
The insurance verification specialists at AcupBilling typically handle these eligibility checks by phone. We prefer speak to a human representative, as automated systems do not always provide complete or reliable information. However given the impact of COVID, phone checks may not be possible. If a check is performed through an online portal, screenshots will be provided.
Once a verification is requested, we will call the insurance company to verify patients benefits within 2 business days.
For new patients, we collect and verify insurance information when they make an appointment. This gives you time to check the information in advance and let the patient know what they’re expected to pay to avoid any unhappy surprises.
For existing patients, insurance benefits should be verified at least once per year when the insurance plan renews or changes, though ideally they should be verified before each visit in order to get up to date information on number of visits left, deductible amounts etc. We make it easy for you to let us know when it’s time to re-check an existing patient’s benefits.
You get notified each time a check is made, directly on the dashboard. At first glance, you are able to see the number of Verified, Incomplete or Pending inquiries sent to us, with a descriptive text for each and direct links to patient files.
Once a verification is completed by a verification specialist, the information will immediately appear in three places:
- In the patient’s file under the “Insurance Tab”
- On the dashboard in the Insurance Verification section (see ‘How am I notified when a check is made?’ FAQ above)
- In the reports section in a report called “Insurance Verification.” For full visibility on all checks, we advise you check this report daily for updates
Insurance is verified based on each clinic’s specific needs. We adapt the questions to best fit your clinic’s insurance billing workflow and can check up to 5 CPT codes per service.
Examples of the questions we ask include:
- Does the patient have acupuncture (or other services) coverage?
- If YES, what are the benefits?
- We inquire about DED, OOP, co-insurance, visits, copay, plan year or calendar year, effective date/end date, DX restrictions, whether pre-authorization is required, etc
Ready to get started?
Simply turn on the Insurance Verification on your Subscriptions Page to accept insurance with peace of mind. When you turn on the service you will be asked to fill out a questionnaire so that we how to best verify insurance benefits for your clinic. The form should take about 5-10 minutes to complete. If you have any questions please reach out to our support team.
